Application of brain research in prescribing antidepressants successful
Nijmegen, January 26, 2021 – The success rate of antidepressants in the treatment of depression can be greatly improved thanks to the use of a short brain examination (EEG) prior to treatment. A study conducted in the Netherlands examined, for the first time, the use of EEG as a biomarker in practice.
read more...
Beyond the 'one-size-fits-all' approach
Until now, the choice for a specific antidepressant was mainly made based on experience and estimation of the prescribing physician. The probability of successful treatment is known to be 30-40%, yet there are dozens of different antidepressant treatments with different mechanisms of action. As a result, it can often take up to three or four different courses of treatment before a patient responds adequately. The use of biomarkers, and therefore measurable predictability, greatly increases the effectiveness of treatment, and can lead to a patient receiving the antidepressant that works for them sooner, as opposed by a trial-and-error approach. This is a major step toward biomarker-based stratified psychiatry.
Scientific breakthrough
Researchers from Synaeda Psycho Medical Center and Research Institute Brainclinics, in collaboration with Amsterdam UMC, Twente University and Duke University (North Carolina, USA), have developed an algorithm that can accurately predict the effectiveness of the three most commonly prescribed antidepressants per individual. By applying this algorithm in practice, the researchers saw that the chance of full recovery (remission) almost doubled, compared to treatment as prescribed by the psychiatrist. This is the very first study worldwide to show that brain activity is a better predictor than the diagnosis of 'depression' per se as applied in practice.
How was the study conducted?
In 195 outpatients with major depressive disorder, a brief brain examination, or EEG, was administered 8 weeks prior to treatment with antidepressants. This group was divided into two groups: 108 of them received a treatment based on the outcome of the EEG examination (thus using the biomarkers found), and the remaining 87 patients received the usual treatment (Treatment As Usual). The outcomes were then compared.
Publication
The results of the study are published in the leading journal European Neuropsychopharmacology.
[custom-twitter-feeds]
News archives
improved succesrate of antidepressants
Application of brain research in prescribing antidepressants successful
Nijmegen, January 26, 2021 - The success rate of antidepressants in the treatment of depression can be greatly improved thanks to the use of a short brain examination (EEG) prior to treatment. A study conducted in the Netherlands examined, for the first time, the use of EEG as a biomarker in practice.
Beyond the 'one-size-fits-all' approach
Until now, the choice for a specific antidepressant was mainly made based on experience and estimation of the prescribing physician. The probability of successful treatment is known to be 30-40%, yet there are dozens of different antidepressant treatments with different mechanisms of action. As a result, it can often take up to three or four different courses of treatment before a patient responds adequately. The use of biomarkers, and therefore measurable predictability, greatly increases the effectiveness of treatment, and can lead to a patient receiving the antidepressant that works for them sooner, as opposed by a trial-and-error approach. This is a major step toward biomarker-based stratified psychiatry.
Scientific breakthrough
Researchers from Synaeda Psycho Medical Center and Research Institute Brainclinics, in collaboration with Amsterdam UMC, Twente University and Duke University (North Carolina, USA), have developed an algorithm that can accurately predict the effectiveness of the three most commonly prescribed antidepressants per individual. By applying this algorithm in practice, the researchers saw that the chance of full recovery (remission) almost doubled, compared to treatment as prescribed by the psychiatrist. This is the very first study worldwide to show that brain activity is a better predictor than the diagnosis of 'depression' per se as applied in practice.
How was the study conducted?
In 195 outpatients with major depressive disorder, a brief brain examination, or EEG, was administered 8 weeks prior to treatment with antidepressants. This group was divided into two groups: 108 of them received a treatment based on the outcome of the EEG examination (thus using the biomarkers found), and the remaining 87 patients received the usual treatment (Treatment As Usual). The outcomes were then compared.
Publication
The results of the study are published in the leading European Neuropsychopharmacology.
Seasonal influence on clinical response to Ritalin in ADHD
Seasonal influence on clinical response to Ritalin in ADHD
Nijmegen, November 25th 2019 – A large global study in which researchers from Research Institute Brainclinics in Nijmegen, Utrecht University and Leiden University collaborated with scientists in the United States and Australia has revealed a surprising insight: how well patients with ADHD respond to treatment with Ritalin seems to depend on the season in which treatment starts. This probably depends on changes in sunlight that affect the biological clock.
Sunlight intensity has a major influence
The researchers involved had previously discovered that ADHD is relatively rare in areas with a lot of sunlight, such as California, Spain and Italy. When sunlight reaches the retina, the internal biological clock receives information about the time of day, and the biological clock runs synchronously with actual clock time. When darkness sets in, the pineal gland starts to produce more melatonin (the "night hormone"). If melatonin production is delayed, people will have more difficulty falling asleep. This specific ‘late circadian phase’ is highly prevalent in patients with ADHD, causing them to have difficulty falling asleep on time, and thereby miss 1-2 hours of sleep every night. Missing 1-2 hours of sleep for a sustained period of time often results in inattentive problems, a feature typically seen in ADHD.
Current study
According to previous research, methylphenidate (the active ingredient in, for example, Ritalin and Concerta) can influence the biological clock. That is why the researchers looked at annual seasonal variation in inattentiveness before and after treatment with methylphenidate, using data from a large international multicenter drug study (iSPOT-A). Locations from both the northern hemisphere (the Netherlands and the US) as well as the southern hemisphere (Australia) took part in this study, whereby the results could be even more convincingly linked to seasonal changes in sunlight.
The results interestingly showed that patients treated with a low-dose methylphenidate during the shortening of days (especially in autumn) showed the same improvement on inattentiveness as seen in patients treated with a high-dose. This effect disappeared when days prolonged - mainly in spring, only patients treated with a high-dose showed a greater improvement in inattentiveness relative to the low-dose.
Conclusion
These results once again demonstrate the important role of the biological clock, sunlight and adequate sleep in inattention, as seen in ADHD. These results also provide more insight into the mechanism-of-action of methylphenidate, the active ingredient of Ritalin, not only as a 'psychostimulant', but also as a treatment that makes the biological clock more sensitive. In addition, the results suggest that low-dosed treatment with methylphenidate suffices in autumn, since the added effect of high-dose was only seen in spring. Possible implications of these results are whether optimal lighting conditions can potentiate the effect of Ritalin, but also what the role of non-pharmacological treatments aimed at sleep and the biological clock could mean, such as light therapy and neurofeedback.
Also see: this informative article on our website (in Dutch).
References:
Madelon A. Vollebregt, J. Leon Kenemans, Jan K. Buitelaar, Tom Deboer, Sean Cain, Donna Palmer, Glen R. Elliott, Evian Gordon, Kamran Fallahpour, Martijn Arns (2019) Annual variation in attentional response after Methylphenidate treatment. doi.org/10.1007/s00787-019-01434-1
Arns, M., van der Heijden, K. B., Arnold, L. E., & Kenemans, J. L. (2013). Geographic variation in the prevalence of attention-deficit/hyperactivity disorder: The sunny perspective. Biological Psychiatry.doi:10.1016/j.biopsych.2013.02.010
The Circadian Phenotype of ADHD explained; an Infographic
circadian rhythms
circadian rhythm infographic
Brainclinic's Martijn Arns and Madelon Vollebregt will present a poster showing the latest insights into the circadian phenotype of ADHD at the EUNETHYDIS conference in Nijmegen on Thursday, September 19, 2019
The Circadian Phenotype of ADHD explained; an Infographic
Vollebregt, M.A., Koppenberg, M., Arns, M.
circadian rhythms
Daylight is the strongest synchronizer of human circadian rhythms. When daylight reaches the retina, it provides the internal clock system [suprachiasmatic nuclei (SCN)] with information about the time of day, thereby leading to daylight entrainment. Even modest misalignment of the internal clock from sleep/wake behavior can result in poorer sleep quality. The circadian pathway hypothesis posits that synchrony between daylight and the circadian system relates to (in)attention. Sleep onset insomnia (SOI) or Delayed sleep phase disorder, a circadian rhythm sleep–wake disorder, is highly prevalent in 73–78% of children and adults with Attention-deficit/hyperactivity disorder (ADHD). Phase-delaying effects can be counteracted by intense natural light in the morning, when our circadian clock is most sensitive to entrainment to the 24h rhythm. Exposure to intense natural light in the morning is more common in geographic areas characterized by high sunlight intensity. Corroboratively, prevalence rates of ADHD are lower in these areas compared to those with less sunlight intensity. The dopamine neurotransmitter system is implicated in regulating the circadian system as well as in ADHD. We demonstrate the role of functional genetic variation in the gene encoding of dopamine-receptor-D4 (DRD4) in the relationship between inattention and seasonal daylight (changes). We also show indications that appropriate lighting could potentiate the effects of stimulants.
References
Vollebregt M.A., Franke B., Buitelaar J.K., Arnold L.E., Faraone S.V., Grevet E.H., Reif A., Zayats T., Bralten J., Bau C.H.D., Haavik J., Kuntsi J., Cupertino R.B., Loo S.K., Lundervold A.J., Ribasés M., Sánchez-Mora C., Ramos-Quiroga, J.A., Asherson P., Swanson J.M., Arns M.. The Role of Gene Encoding Variation of DRD4 in the Relationship between Inattention and Seasonal Daylight. Under review in Neuropsychopharmacology.
Vollebregt M. A., Arns M., Monastra V., Roley-Roberts M. E., Arnold L. E., & Hollway J. A. (2019a, June 12). Shedding light on the etiology of ADHD: The influence of disturbed sleep on symptomatology.
Vollebregt M. A., Kenemans J.L., Buitelaar J.K., Deboer T., Cain S., Palmer D., … Arns M. (2019b, June 12). Annual variation in attentional response after Methylphenidate treatment. In revision in European Child & Adolescent Psychiatry
Bijlenga, D., Vollebregt, M. A., Kooij, J. J. S., & Arns, M. (2019). The role of the circadian system in the etiology and pathophysiology of ADHD: Time to redefine ADHD? Attention Deficit and Hyperactivity Disorders, 11(1), 5-19. doi:10.1007/s12402-018-0271-z
Arns, M., & Vollebregt, M. A. (2019). Editorial: Time to wake up: Appreciating the role of sleep in attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 58(4), 398-399.
Arns, M., Swanson, J. M., & Arnold, L. E. (2015). DHD prevalence: Altitude or sunlight? Better understanding the interrelations of dopamine and the circadian system. Journal of Attention Disorders. doi:10.1177/1087054715599574
Arns, M., Feddema, I., & Kenemans, J. L. (2014). Differential effects of theta/beta and SMR neurofeedback in ADHD on sleep onset latency.. Frontiers in Human Neuroscience, 8, 1019. doi:10.3389/fnhum.2014.01019
Arns M., van der Heijden K.B., Arnold L.E. & Kenemans J.L. (2013): Geographic variation in the prevalence of attention-deficit/hyperactivity disorder: The sunny perspective. Biological Psychiatry: DOI: 10.1016/j.biopsych.2013.02.010
Arns, M. & Kenemans, J.L. (2012). Neurofeedback in ADHD and insomnia: Vigilance Stabilization through sleep spindles and circadian networks. Neuroscience and Biobehavioral Reviews 183-194. doi: 10.1016/j.neubiorev.2012.10.006
biomarker bij depressie
Kort hersenonderzoek maakt passende behandeling van depressie mogelijk en vergroot snelle kans van slagen
Nijmegen, 6 september, 2019 - Een eenvoudig en kort EEG-onderzoek kan een belangrijk hulpmiddel zijn bij het voorschrijven van de juiste medicatie bij depressieve klachten, blijkt uit een nieuw onderzoek van Nikita van der Vinne en collega’s in het Journal of Affective Disorders.
Biomarkers als richtingaanwijzer bij behandeling
Doorgaans worden patiënten met depressieve klachten behandeld met antidepressiva zoals escitalopram, venlafaxine of sertraline. De behandelend psychiater maakt, bijvoorbeeld op basis van ervaring, de keuze met welk antidepressivum gestart wordt. Als er een meetbare indicator ofwel biomarker zou bestaan waarmee meer objectief voorspeld kan worden of een middel zal aanslaan of niet, zouden patiënten daar enorm veel baat bij kunnen hebben. Het zou er namelijk voor kunnen zorgen dat de eerste behandelpoging meteen aanslaat in plaats van pas een latere poging. Uit het onderzoek van Nikita van der Vinne blijkt dat zo’n marker bestaat.
Van der Vinne ontdekte, samen met wetenschappers van Onderzoeksinstituut Brainclinics, Universiteit Twente, en uit de VS (Kansas en New York), lichte afwijkingen in de EEG’s van een kleine groep depressieve patiënten. Wanneer deze lichte afwijkingen na behandeling niet meer gemeten werden, bleken deze patiënten 5 keer vaker gunstig te hebben gereageerd op behandeling met sertraline dan op behandeling met escitalopram of venlafaxine. Dit suggereert dat deze specifieke subgroep van depressieve patiënten wellicht de grootste kans van slagen van behandeling heeft wanneer sertraline voorgeschreven wordt.
Het gebruiken van een EEG als biomarker brengt precisiegeneeskunde dichterbij
Martijn Arns van Brainclinics: “In de psychiatrie wordt met name gekeken naar gedrag om vervolgens een ‘biologische’ behandeling zoals medicatie toe te passen, terwijl het eigenlijk logischer zou zijn om eerst naar het functioneren van de hersenen te kijken, net zoals cardiologen al jaren hartfilmpjes maken alvorens tot behandeling over te gaan.”
De uitkomst van Van der Vinnes onderzoek is een belangrijke stap in de richting van gestratificeerde geneeskunde, waarbij behandelkeuze geïnformeerd wordt door specifieke kenmerken van subgroepen uit de te behandelende populatie, “…omdat we nu een subgroep kunnen identificeren binnen het totaal van alle patiënten met depressieve klachten kunnen we die nu gerichter gaan behandelen, hetgeen leidt tot een snellere positieve uitkomst bij deze patiën-ten.” aldus Van der Vinne. Zij en haar collega’s onderzoeken ook andere biomarkers om zo gerichte behandelkeuzes te kunnen maken voor meerdere subgroepen van depressieve patiënten.
Nikita van der Vinne is momenteel werkzaam als neuropsycholoog-onderzoeker bij Synaeda Psycho Medisch Centrum in Leeuwarden, waar ze in samenwerking met Onderzoeksinstituut Brainclinics de nieuwste kennis op het gebied van gestratificeerde behandeling van depressie implementeert in de praktijk, als onderdeel van haar promotieonderzoek aan de Universiteit Twente.
Referenties:
van der Vinne, N., Vollebregt, M.A., Boutros, N.N., Fallahpour, K., van Putten, M.J.A.M., Arns, M. (2019). Normalization of EEG in depression after antidepressant treatment with sertraline? A preliminary report. Journal of Affective Disorders, 259 (2019) 67-72. doi:10.1016/j.jad.2019.08.016
Arns, M., Gordon, E., & Boutros, N.N. (2017). EEG abnormalities are associated with poorer depressive symptom outcomes with escitalopram and venlafaxine-XR, but not sertraline: Results from the multicenter randomized iSPOT-D study. Clinical EEG and Neuroscience, 48(1), 33-40. doi:10.1177/1550059415621435
consensusverklaring
Paradigmaverschuiving binnen de psychiatrie: Standaarden voor magnetische hersenstimulatie bij depressie
Nijmegen, 18 juni 2019 –Na meer dan 30 jaar onderzoek naar transcraniële magnetische hersenstimulatie (rTMS) bij de behandeling van depressie, dringt deze techniek steeds verder door in de psychiatrische en psychologische behandelpraktijk. Om die reden hebben verschillende onderzoekers en instanties (waaronder Onderzoeksinstituut Brainclinics, NedKAD en de hersenstimulatiestichting) zojuist een consensusverklaring gepubliceerd in het tijdschrift voor psychiatrie. Deze verklaring dient ter verduidelijking van de rol en plek van magnetische hersenstimulatie bij de behandeling van depressie maar ook als handvat om deze techniek effectief en veilig toe te passen.
Noodzaak: de ontwikkeling van nieuwe antidepressiva stagneert.
Sinds 2010 investeren de meeste farmaceutische bedrijven niet meer in de ontwikkeling van nieuwe antidepressiva, waardoor er grote behoefte is aan nieuwe en effectievere behandelingen van depressie.
Magnetische hersenstimulatie: Een paradigmawisseling binnen de psychiatrie?
Binnen de psychiatrie wordt de techniek van transcraniële magnetische hersenstimulatie (rTMS) al sinds 1985 intensief onderzocht. Deze techniek is onderdeel van een bredere ontwikkeling binnen de psychiatrie, waarbij steeds meer aandacht is voor ‘neuromodulatie’ technieken, waarbij hersenactiviteit veel gerichter beïnvloed kan worden, vaak met minder bijwerkingen in vergelijking met medicatie. Voorbeelden van deze neuromodulatie technieken zijn onder andere diepe hersenstimulatie bij Parkinson, dwang en depressie, maar ook rTMS.
Het duurt vaak lang voordat dit soort nieuwe ontwikkelingen doordringt in de psychiatrische en psychologische behandelpraktijk, te vergelijken met de trage adoptie van de elektrische auto, en dit wordt binnen de psychiatrie dan ook gezien als een paradigmaverschuiving.
rTMS bij depressie en consensusverklaring
Dr. Martijn Arns is sinds 2006 één van de pioniers die zich heeft toegelegd op de toepassing en vooral verfijning en optimalisatie van de transcraniële magnetische hersenstimulatie techniek (rTMS), bij met name de behandeling van depressie. Sinds medio 2017 is deze behandeling ook erkend als vergoede zorg door Nederlandse zorgverzekeraars, waardoor meer patiënten profijt kunnen hebben van deze behandeling.
De belangrijkste conclusie van de consensusverklaring is dat rTMS een bewezen effectieve en veilige behandeling bij depressie is, met gunstige lange termijneffecten, mits de behandeling met rTMS wordt uitgevoerd onder supervisie van een (BIG) geregistreerde psycholoog of psychiater, waarbij de bekende veiligheidsrichtlijnen in acht worden genomen.
Martijn Arns: “Om die reden heeft een groep van onderzoekers van verschillende instanties en universiteiten, waaronder Onderzoeksinstituut Brainclinics, NedKad en de Hersenstimulatiestichting, de handen ineengeslagen om tot een eerste consensusverklaring te komen voor een veilige, verantwoorde en effectieve toepassing van rTMS bij de behandeling van depressie. Voor de kwetsbare patiëntgroepen die behandeld kunnen worden met rTMS is deze verklaring enorm belangrijk: het is een eerste aanzet tot standaardisering en kwaliteitsbewaking van (medisch) verantwoord handelen.”
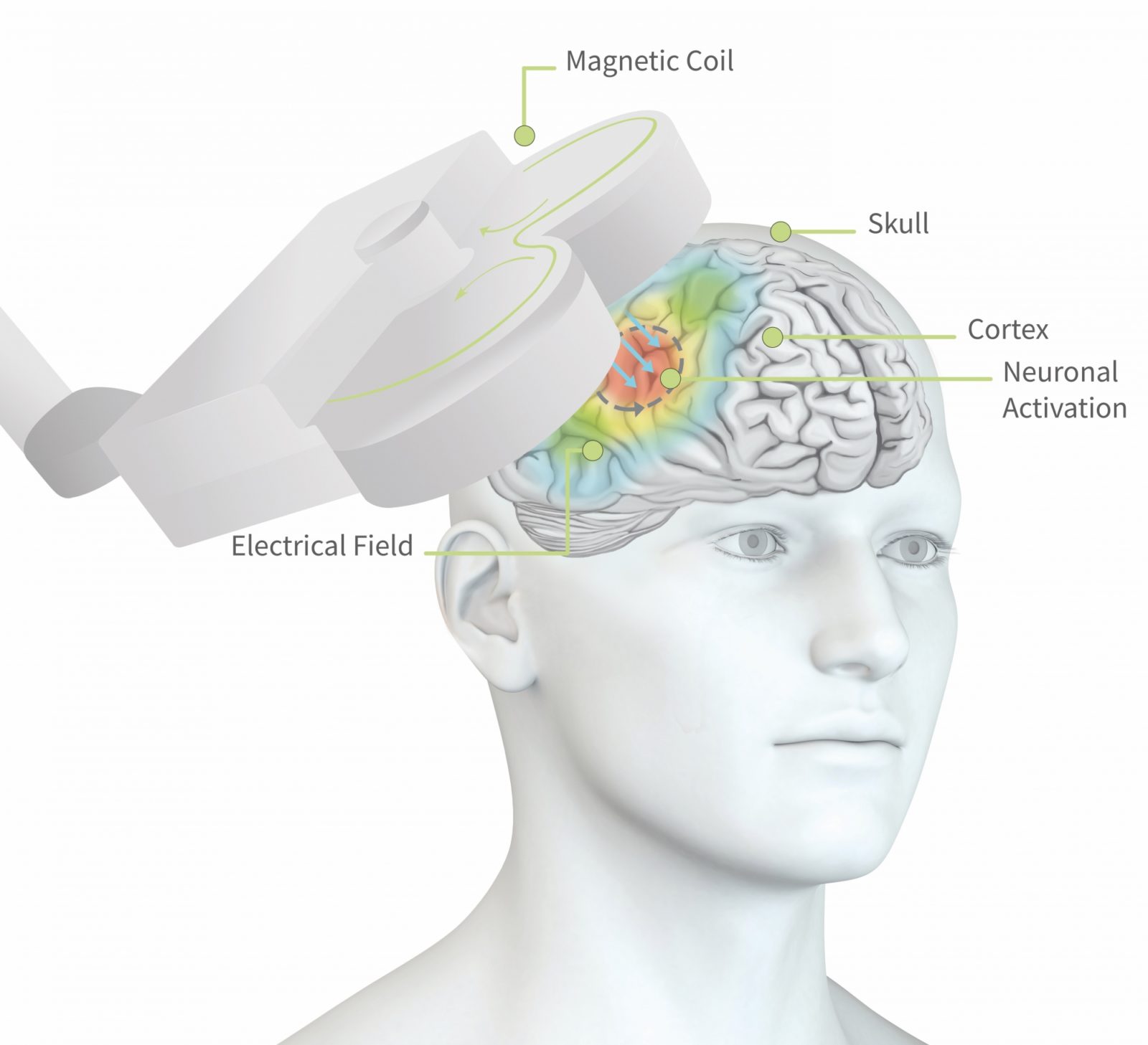
Hoe werkt rTMS?
(repetitieve) Transcraniële magnetische stimulatie (rTMS) is een niet-invasieve en medicatie-vrije behandelmethode bij depressie. Een spoel die geplaatst wordt op het hoofd genereert een pulserend magnetisch veld en stimuleert specifieke gebieden van de hersenen die betrokken zijn bij depressie.
Na ongeveer 10 – 15 behandelsessies kunnen de eerste positieve effecten al waarneembaar zijn. In combinatie met psychotherapie kan dit effect worden versterkt en gestabiliseerd.
De behandeling is een precies gerichte, milde en veilige, effectieve therapie. Over het algemeen wordt de magnetische stimulatie niet als pijnlijk ervaren, maar een bijwerking van rTMS die soms voorkomt is lichte hoofdpijn. Deze wordt veroorzaakt door het samentrekken van spieren rondom hals, nek en hoofd en verdwijnt na korte tijd vanzelf.
rTMS is geschikt voor mensen met een depressie of behandelresistente depressie. rTMS werd voor het eerst succesvol toegepast in 1985. Sinds die tijd is de techniek uitgebreid onderzocht en steeds verder geperfectioneerd.
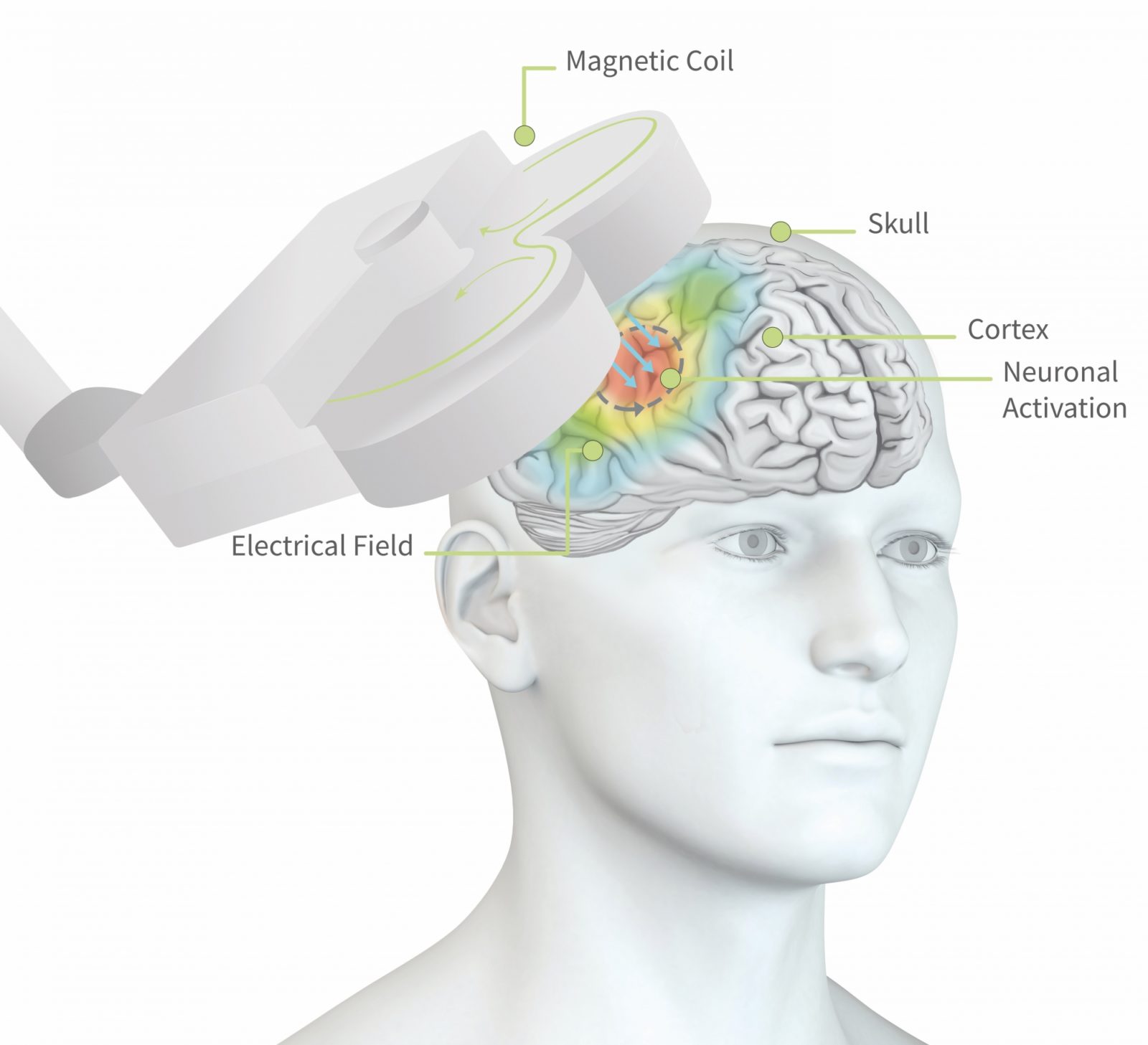
Figuur 1: de pulsen uit de magneetspoel dringen tot ca. 2cm diep in de hersenen door en stimuleren lokale hersencellen tot actie. Dit kan ervoor zorgen dat het groepje hersencellen, of het netwerk dat daaraan vast zit, geactiveerd wordt.
Referenties:
1)Arns, M., Bervoets, C., van Eijndhoven, P., Baeken, C., van den Heuvel, O. A., Aleman, A., . . . Sack, A. T. (2019). Consensusverklaring voor de toepassing van rTMS bij depressie in Nederland en België. Tijdschrift Voor Psychiatrie, 61(6), 411-420.
2) Donse, L., Padberg, F., Sack, A. T., Rush, A. J., & Arns, M. (2017). Simultaneous rTMS and psychotherapy in major depressive disorder: Clinical outcomes and predictors from a large naturalistic study. Brain Stimulation.doi: https://doi.org/10.1016/j.brs.2017.11.004
Lees de consensusverklaring
Zeven voor leven
Sponsoring groot succes
Het Brainclinics-Vidacto team droeg ruim duizend euro bij aan het totaal van €167.612,- dat de Zeven voor Leven sponsorrit bijeenbracht voor de Stichting Kanker Zien. Na afloop van de sponsorrit spraken we kort met Martijn Arns, oprichter van Brainclinics en ploegleider van het wielerteam.
Gefeliciteerd met jullie prestatie! Hoe ging het?
Dankjewel! Het viel 100% mee. De rit zelf was best stevig, 140 kilometer in totaal, en door het hoogteverschil van het parcours hebben we 2000 meters geklommen. De moraal was goed en bleef dat ook.
Hoe hoog eindigden jullie in het klassement?
Het mooie van de Zeven voor Leven sponsorrit is dat iedereen eigenlijk een winnaar is. De renners, die naar hun eigen maatstaf kunnen presteren, de sponsors, omdat ze bijdragen aan goed en belangrijk onderzoek naar het herkennen van kanker in een vroeg stadium, de Stichting Kanker Zien, omdat ze met een eerste sponsorrit al ruim 167.000 euro binnenhalen, en natuurlijk de (toekomstige) kankerpatiënten, die een betere overlevingskans in het vooruitzicht hebben.
Je noemt presteren naar je eigen maatstaf, wat bedoel je daarmee?
Een ronde is ongeveer 20 kilometer, en je kunt maximaal 7 ronden rijden. Maar omdat het sponsorbedrag niet verbonden is aan het aantal ronden dat je rijdt kan je ook minder ronden rijden en toch een vol bedrag binnenfietsen. Daardoor is meedoen eigenlijk belangrijker dan winnen, of veel kilometers maken. Ik ben blij met onze prestatie, we hebben met het team de zeven ronden volgemaakt en daarbij een goed gemiddelde gereden. En we hebben ruim duizend euro binnengebracht!
Volgend jaar weer?
Wie weet wat de toekomst brengt!

foto: Abigaël de Vries


Team Brainclinics-Vidacto. vlnr: Noud van Hecke, Bas Vroemen, Martijn Arns
The relationship between sleep and ADHD
Nijmegen, April 23rd, 2019 - Dutch researchers from Research Institute Brainclinics in Nijmegen and PsyQ, (Kenniscentrum ADHD bij volwassenen) in The Hague, discovered a striking link between light, sleep and ADHD, as can be read in two recent scientific publications. They published a study showing that ADHD can be a cause or a consequence of a disturbed sleep-wake rhythm. This new insight can be of great importance in the treatment of ADHD.
The importance of sleep
Three out of four adults and children (± 75%) with ADHD have difficulty falling asleep.
This sleep-wake disorder has major consequences for health, concentration and daily functioning: if you lie awake longer, you wake up less refreshed the next day, fatigue increases, and your school or work performance and concentration diminishes.
Circadian rhythm and sleep pressure
The orange line in Figure 1 shows how fatigue increases during the day. After you have slept, tiredness decreases. This is called sleep pressure. Ideally, sleep pressure and the biological clock are in sync.
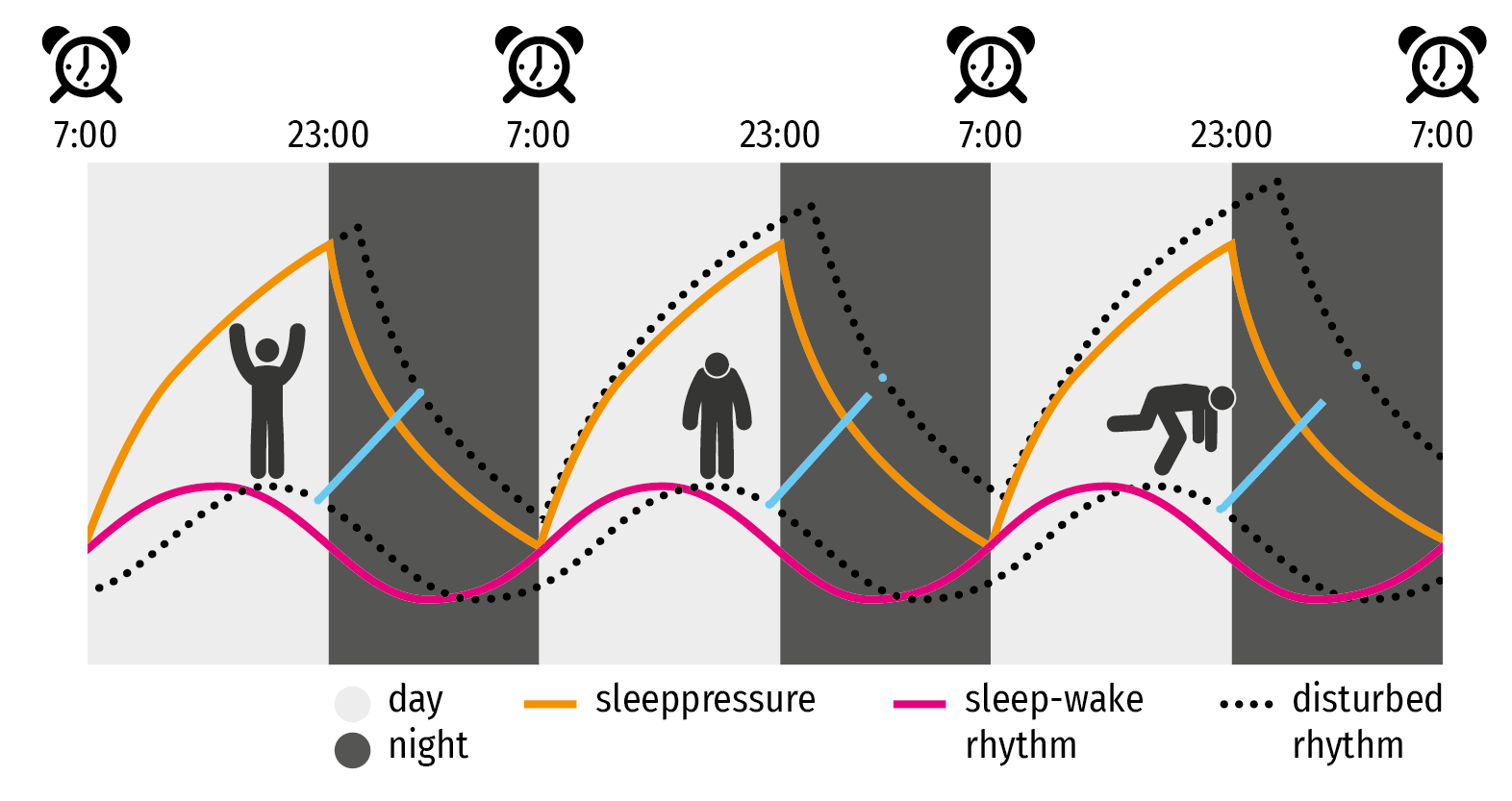
Figure 1: Circadian rhythm: With normal sleep, the ratio between sleep pressure (orange line) and circadian rhythm, also called biological clock, (pink line) is optimal. With a delayed rhythm, these processes increasingly grow further apart (blue lines): it becomes more difficult to fall asleep, and fatigue increases faster during the day.
How the circadian rhythm can be disturbed
Melatonin, the "sleep hormone", plays an important role in regulating the sleep-wake rhythm. The amount of melatonin your body releases is determined by the amount of daylight exposure. At the end of the day, when daylight decreases, you release more melatonin that makes you more sleepy assuming disturbing factors play no role. The use of modern media can be considered such a disturbing factor. Tablet and smartphone screens, but also LED lights, radiate blue light that falls in the same spectrum as daylight.If you use those in the evening, the body will postpone and lower the production of melatonin. The result: you will fall asleep later (sleep delay), and because your alarm clock (due to daily obligations) goes off at a regular time, you effectively sleep fewer hours.
The consequences of a (too) short night's rest (sleep restriction) are often underestimated, but the result of a few hours' missed sleep every night is comparable to staying awake for 48 hours (sleep deprivation), with all the associated negative effects. While the adverse effects of sleep deprivation are well known, with sleep restriction people are not aware of the same symptoms (for example, reduced concentration and vigilance).
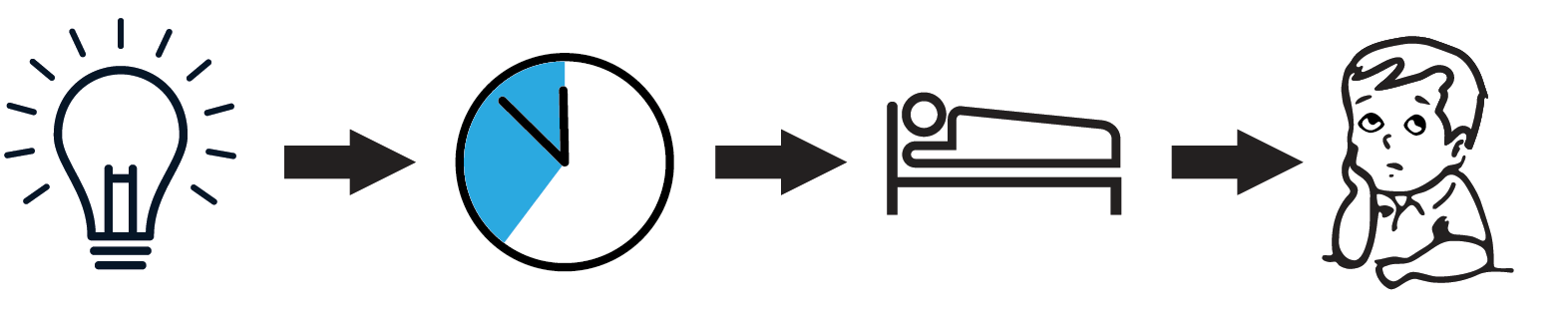
Figure 2: Consequence of exposure to blue light just before going to sleep: A pathway is depicted in which LED light exposure results in a sleep-onset delay, which in turn negatively influences the amount of time spent sleeping, which ultimately leads to worsening of attention.
Sleep problem as a cause and effect of ADHD
The functional and neuro anatomical overlap between brain areas involved in attention, alertness and sleep regulation reflects the complex relationship between ADHD and sleep.
A sleep problem can be either cause, effect or intrinsic characteristic of ADHD. An example: young children who are very tired become very energetic. Here, drowsiness is the cause of hyperactivity. However, ADHD can also be the cause of problems falling asleep: for example, problems with inner unrest, grinding, or pressure in the head. It could also be that ADHD and sleeping problems both stem from the same underlying problem.
Similarities between ADHD and sleep disorders
There are many similarities between the symptoms of ADHD and those of sleep disorders: problematic behavior, learning disabilities, concentration problems and emotion disorder, and often the symptoms of ADHD exacerbate the sleep problem, or vice versa. Symptoms of ADHD, a delayed circadian rhythm and sleep disorders are therefore intertwined. They seem to share a genetic and etiological background and can benefit from a common treatment.
How do you resolve sleeping problems?
Sleep problems related to mood or anxiety disorders can be reduced by addressing the causes. Sleep problems due to a chaotic lifestyle, which is generally a characteristic of ADHD, can be reduced by the medical and psychological treatment of ADHD itself. Improved sleep hygiene (no tablet or smartphone use in the hours before bedtime, no coffee in the evening, regular bedtimes) is very important. The preferred treatment for insomnia is a cognitive behavioral treatment (CBTi), which focuses on good sleep hygiene, good bed-sleep association and relaxation training, among other things. CBTi has been proven to be very effective for symptoms of insomnia and sleep quality improvement, is safe, has no side effects and is therefore preferable to sleep medication. Chronotherapy, for example through the administration of light therapy or melatonin, certainly has a positive effect on children with ADHD in the longer term, as has neurofeedback.
ADHD-SOM
Improving sleep quality has a favorable effect on ADHD symptoms and it is therefore advisable to include such a focus in ADHD treatments. In addition, the term ADHD is too general: because ADHD is so often associated with sleeping problems, the authors propose to create a separate DSM-5 classification for this category: ADHD-SOM (derived from somnus, or sleep), which enables specialists to propose a much more focused and personalized treatment.
References:
Bijlenga, D. Vollebregt, M.A. Kooij, J.J.S Arns, M. (2019) The role of the circadian system in the etiology and pathophysiology of ADHD: time to redefine ADHD?ADHD Attention Deficit and Hyperactivity Disorders DOI: 10.1007/s12402-018-0271-z
Arns, M. Vollebregt, M.A. (2019) Time to Wake Up: Appreciating the Role of Sleep in Attention-Deficit/Hyperactivity DisorderJournal of the American Academy of Child and Adolescent Psychiatry Vol.58 Number 4 April 2019 DOI: 10.1016/j.jaac.2018.10.013
racing against cancer
Nijmegen, 19 April 2019 - Brainclinics and Vidacto join forces to race towards a cancer-free future!
Zeven voor Leven (Seven for Life)
May 26, 2019, the cycling challenge Zeven voor Leven (Seven For Life) will be held for the first time in the hilly landscape around the municipality of Berg en Dal. The proceeds of the cycling round will go entirely to the Stichting Kanker Zien (Spot Cancer Foundation). The foundation wants to be able to diagnose cancer at an earlier stage and treat tumors in a more targeted way. This also improves the quality of life after treatment. The foundation even strives for complete prevention of this disease.
Frits Barend, Tim de Vries and Team Sunweb have committed themselves as ambassadors to Zeven voor Leven.
Trail
The trail is 20 km long and leads, among other things, along the Zevenheuvelenweg. The challenge is to complete the round seven times. During those 140 kilometers, around 2000 altimeters are made together. The start and finish take place at the Ketelwoud event site.
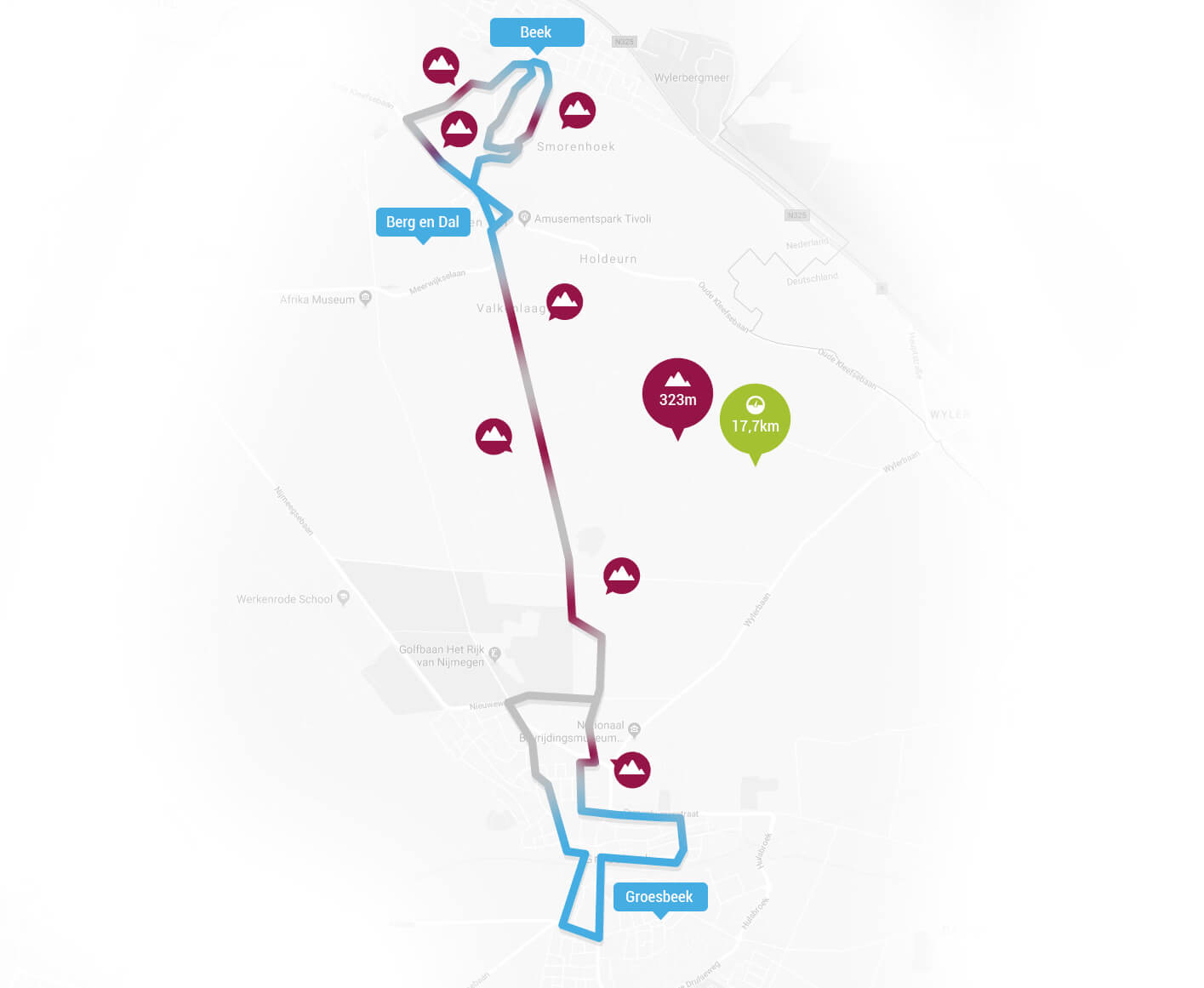
Route (subject to change)
Team Brainclinics-Vidacto
Team Brainclinics-Vidacto stands for health and vitality, and it is therefore a no-brainer for us to participate and thus contribute to this charity.
You can sponsor the Stichting Kanker Zien by visiting our team page and sponsoring us. In this way we all cycle to a future where cancer can be prevented!

Together towards a future in which cancer can be prevented!
Brain activity predicts response to Ritalin in ADHD
Brain activity predicts response to Ritalin in ADHD; Implications for male-female differences
Nijmegen, July 3rd, 2018 – Today results from the large multicenter iSPOT-A study were published in European Neuropsychopharmacology, demonstrating that brain activity can assist in predicting response to Ritalin in male adolescents with ADHD. In addition, this study clearly demonstrated gender differences in brain activity, where brain activity only predicted Ritalin response in males and not in females with ADHD. No differences in brain activity were found between children with and without ADHD, further demonstrating the value of brain imaging in prognosis rather than diagnosis.
An international group of researchers including researchers from Research Institute Brainclinics, Brainresource, University of Sydney, Utrecht University, Stanford School of Medicine, Westmead Hospital and Radboud University Nijmegen published results from the international multicenter iSPOT-A study (international Study to Predict Optimized Treatment in ADHD). This study recruited 336 children and adolescents with ADHD who were subsequently treated with methylphenidate and 158 children and adolescents without ADHD, and is the largest brain imaging study in ADHD focused on predicting response to Ritalin. Researchers measured brain electrical activity, also called EEG or QEEG before treatment and clinical measures before and after treatment. When looking at differences in brain activity between participants with and without ADHD, no differences in brain activity were found. However, a clear difference was found between adolescents that did and did not respond to treatment with methylphenidate, albeit only for males, suggesting sex specific differences in the etiology of ADHD.
Predicting Ritalin response in ADHD
The main aim of the study was to investigate if brain-based ‘biomarkers’, such as measured with QEEG, could predict treatment response. This study demonstrated that a single biomarker –
namely Alpha Peak Frequency (APF) – was able to predict treatment response to methylphenidate for male adolescents. This study replicates and extends an earlier pilot-study that already suggested that this biomarker could predict treatment non-response (Arns et al., 2008). “… the most striking aspect of the outcome of the study is that no difference in brain activity as measured using EEG was found between patients with and without ADHD, whereas brain activity was clearly different between male adolescents with ADHD that did and did not respond to methylphenidate, further demonstrating that brain imaging is better used for ‘prognosis’ and not for ‘diagnosis’. This finding offers hope and can prospectively be used to develop new treatments that are specifically aimed at this biomarker…’ said Martijn Arns, first author on the study. This biomarker – possibly used in conjunction with other biomarkers identified in the iSPOT studies – could help assist in a future of Personalized Medicine or Precision Medicine, where biomarkers are used to objectively guide patients to the optimal treatment and can aid in discovery of new treatments aimed at this subgroup.
Reference:
Arns, M., Vollebregt, M.A., Palmer, D., Spooner, C., Gordon, E., Kohn, M., Clarke, S., Elliott, G., Buitelaar J.K. (2018). Electroencephalographic biomarkers of methylphenidate response in Attention- Deficit/Hyperactivity Disorder. European Neuropsychopharmacology. doi: 10.1016/j.euroneuro.2018.06.002
Arns, M., Gunkelman, J., Breteler, M., & Spronk, D. (2008). EEG phenotypes predict treatment outcome to stimulants in children with ADHD. Journal of Integrative Neuroscience, 7(3), 421-38.
Meta-analysis confirms sustained effects of neurofeedback
Meta-analysis confirms sustained effects of neurofeedback in children with ADHD
Nijmegen, February 16th, 2018 - An international group of researchers conducted a meta-analysis that systematically looked at all available studies and found that after an intensive course of neurofeedback, the clinical benefit of neurofeedback on ADHD symptoms was maintained over a 6-month follow-up period (without treatment). At follow-up the effects of neurofeedback were not inferior to active treatments such as medication, whereas benefits for non-active control groups (such as cognitive training) were no longer present at follow-up. These results have now been published in the scientific journal European Child & Adolescent Psychiatry.
Neurofeedback is a treatment where real-time feedback is provided on specific brain activity (most often the EEG) and based on learning principles participants learn to control specific types of brain activity. Based on the notion that this treatment is based on learning principles, it is expected that it should result in long-term benefits, however durability has not been systematically investigated. Given treatment with medication in ADHD is effective in short-term symptom management, and clinical benefit is likely to diminish after sustained use for more than 2 years, there is a need for treatments that result in better long-term benefits. Therefore, an international group of researchers from The Netherlands (Utrecht University, Research Institute Brainclinics, Radboud University), Germany (University Hospital Erlangen; kbo-Heckscher-Klinikum, Tübingen University, neuroCare Group), and the United States (UCLA), conducted a systematic-review and meta-analysis to investigate the long-term effects of neurofeedback and different control groups, including medication. This research group was selected to include scientists with different views on neurofeedback to interpret the data in a balanced and critical manner.
In this study, researchers compiled data of more than 500 children with ADHD comparing the results of neurofeedback, active (incl. medication), and 'non-active' control conditions from 10 randomized controlled studies (RCT's) and clinical benefit was assessed after a follow-up period of on average 6 months after treatment was finished. It was found that neurofeedback resulted in a large effect on inattention and medium effect on hyperactivity/impulsivity at follow-up and at this time-point there were no differences between neurofeedback and active-treatments. For non-active controls a small effect was found only on inattention that disappeared at follow-up. Numerically, the benefits of neurofeedback tended to improve from outtake to follow-up, which was not the case for the other treatments. Furthermore, for the medication groups, medication was still used in the 6 month interval to follow-up, whereas for neurofeedback no additional treatment sessions were administered in that interval.
Concluding, these results suggest that clinical benefits achieved with neurofeedback in children with ADHD have durable effects at least over a 6-month period without treatments, positioning neurofeedback as a promising treatment with long-term benefit.
Note: The results from this meta-analysis mainly apply to the specific protocols investigated and might not generalize to other 'experimental' approaches implemented in many 'neurofeedback clinics'. Currently, there is most consistent evidence for Slow Cortical Potential (SCP), Theta/Beta (TBR) and Sensori-Motor Rhythm (SMR) neurofeedback, see figure below for explanation.
Reference:
Van Doren, J., Arns, M., Heinrich, H., Vollebregt, M. A., Strehl, U., & Loo, S. K. (2018). Sustained effects of neurofeedback in ADHD: A systematic review and meta-analysis. European Child & Adolescent Psychiatry. doi:https://doi.org/10.1007/s00787-018-1121-4
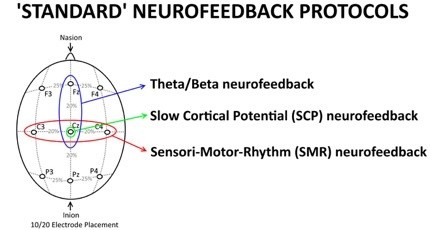
Figure 1 An explanation of 'Standard NF protocols' as a function of training site. Theta/Beta neurofeedback protocols are specifically trained at Fz or Cz, in line with most studies that have assessed the Theta/Beta ratio at those sites; SCP neurofeedback is always applied at Cz and SMR neurofeedback is always applied at a site that overlies the sensori-motor strip, i.e. C3, Cz or C4. Theta/Beta neurofeedback is focused on downtraining Theta and rewarding Beta, SMR is focused on SMR enhancement and SCP neurofeedback is focused on bidirectional training of negativation and positivation. These three protocols have been most investigated in the treatment of ADHD, and most studies included in the meta-analysis employed one of these protocols.
Male and female brain rhythms show differences
Male and female brain rhythms show differences; 'Deep-Learning' reveals different EEG patterns
The electric brain signals, measured by using EEG, of males and females show differences. The difference can’t be detected by visual inspection, not even by the trained eye of a neurologist. A ‘deep learning’ computer is able to find it. Researchers of the University of Twente, the University of Zürich and Research Institute Brainclinics in Nijmegen, publish these results in Scientific Reports of 15 February.
Male and female brains are different, functionally and anatomically. But that the EEG (electro-encephalography) signals, measured using electrodes placed on the skull, show different signals as well, was not demonstrated yet. For the interpretation of EEG signals, advanced pattern recognition techniques have been developed the last decades. Still, in many cases, the trained eye of the neurologist gives better results. Even these trained eyes are not able to recognize a difference between male and female brain rhythms. For this, artificial intelligence, so-called ‘deep learning’, is needed.
Training
The researchers had a large set of over 1300 EEG patterns, from several laboratories, at their disposal. This set has been entered into a learning computer, a so-called ‘convolutional neural network’. This is an artificial neural net existing of several layers and determining over nine million parameters. The network was first trained using 1000 EEG’s of just two minutes, with a known outcome: male or female. This was not a training based on entering specific characteristics, as these were not known beforehand. After training, the computer was fed with an independent set of EEGs. In over 80 percent, the system gives the right answer. This is well above the significance threshold.
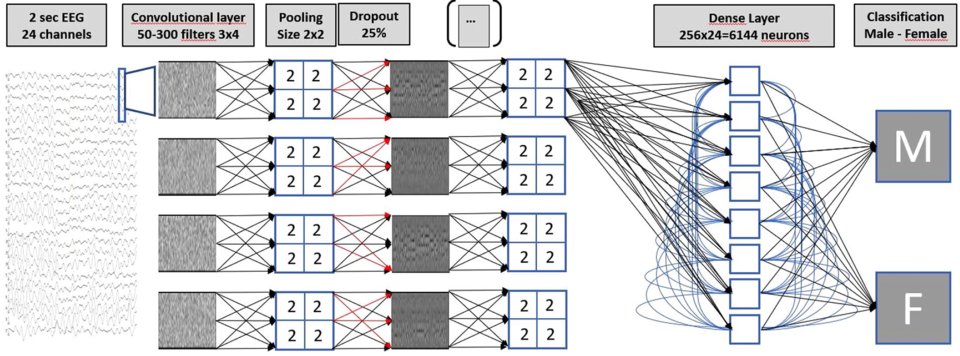
Figure 1 The multilayer neural net setup, used for classifying EEG readings
BETA ACTIVITY
The next step: extract the specific features that make the difference, from the neural net. The main difference is in the ‘beta activity’, a frequency range between 20 and 25 Hz. These rhythms have to do with cognition and with tasks that are emotionally positive or negative. It is known from previous research that females are better capable of recognizing emotion: this could indicate a difference in beta activity. Within the context of this research project, this has not been elaborated further. The outcomes don’t give an answer to transgender issues either.
PERSONALIZED TREATMENT
It seems a complicated way of assessing sex, using EEG and strong computing power. An interesting question, however, can be: do females and males respond to neurological or psychiatric disorders in different ways. And thus: is it, based on this knowledge, possible to better tailor the treatment? Apart from that, this research shows that there is a lot more information inside an EEG than meets the eye. Previous research using the combination of EEGs and deep learning, was on sleep analysis, responds to music or early detection of brain diseases. There is enough reason for further exploring this potential, as it could lead to better insights and personalized treatment.
The research has been done by Michel van Putten, professor of clinical neurophysiology at the University of Twente and neurologist at the Medisch Spectrum Twente hospital in Enschede. He collaborated with Sebastian Olbrich of the Psychiatric clinic of the University of Zürich and with Martijn Arns of Research Institute Brainclinics in Nijmegen. Also see University Twenthe website.
Their paper 'Predicting sex from brain rhythms with deep learning’, is published in ‘Scientific Reports’ of 15 february. This is a Nature publication.
Combined rTMS-psychotherapy effective treatment for depression
Combined rTMS and psychotherapy an effective treatment for depression
Nijmegen (The Netherlands), November, 16th 2017 – Magnetic brain stimulation (rTMS) combined with concurrent psychotherapy seems more effective, then either alone, as was just published in the international journal ‘Brain Stimulation’ based on a study in 196 patients. After an average of 21 sessions, 66% of patients with treatment resistant depression responded well to treatment, with a lasting effect after 6 months in 65% of this group.
rTMS an effective add-on for psychotherapy
A large study by Donse, Padberg, Sack, Rush and Arns 1), carried out in the Netherlands has investigated the effects of combining brain stimulation (rTMS) with concurrent psychotherapy in treatment resistant depression. The study was conducted by Research Institute Brainclinics in collaboration with neuroCare Group. The results of this study suggest that a combined approach is more clinically effective than if either therapy was delivered alone. 66% of the patients in this study responded positively to the combined therapy (i.e. symptom decrease of more than 50%), while 56% of the total sample achieved remission (meaning that they no longer met criteria for depression). Follow-up after 6 months demonstrated that 65% of the patients still had benefit from the initial course of treatment, which suggests that the effects are durable. On average patients received 21 treatment sessions. The results of this study are published this month in the leading international journal: Brain Stimulation.
Studies show that when either rTMS or Psychotherapy are conducted as a monotherapy, an average of 30-40% of patients achieve remission, clearly less than the 56% remission achieved with the combined treatment of rTMS and psychotherapy. Similarly, it is widely known that ‘psychotherapy and drugs’ combined show better outcomes, however this approach often requires two separate treatment programs and specialists, i.e. a Psychiatrist to deliver medications and a Psychologist to deliver Psychotherapy. A combined approach of Psychotherapy at the same time as brain stimulation, can be performed by one clinician and is shown to be more efficient, and above all, a more effective treatment for treatment resistant Depression.
Recognition
The efficacy of rTMS as a monotherapy (i.e. conducted without individual psychotherapeutic support) is recognized throughout the world as a valid treatment for Depression and is furthermore supported by FDA approval in the United States, and is recognized by NICE in the United Kingdom. Since 2011, Health Insurance providers in The United States, and more recently, in The Netherlands, reimburse rTMS treatment for treatment resistant depression.
How does it work, combined rTMS and Psychotherapy?
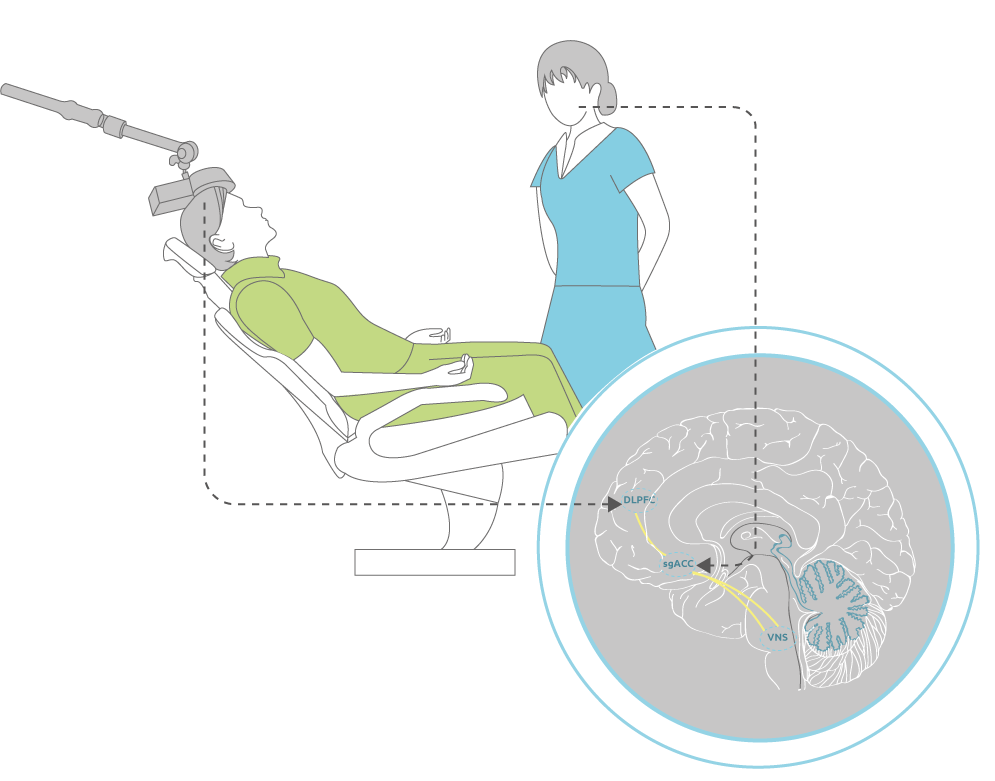
Research has shown that depression is linked to disrupted communication in a specific network of brain structures including the frontal cortex (dorsolateral prefrontal cortex (DLPFC)) and the deeper anterior cingulate (sgACC). rTMS focuses specifically on the DLPFC, whereby indirectly stimulation of the sgACC is also achieved transsynaptically as we demonstrated before using Heart-Brain Coupling 2). For psychotherapy, it is thought that among other areas, it also activates the deeper sgACC in this network more directly. Concurrent application of both techniques thus activates a larger part of this malfunctioning ‘depression network’, with higher clinical efficacy.
References:
>1) Donse, L., Padberg, F., Sack, A. T., Rush, A. J., & Arns, M. (2017). Simultaneous rTMS and psychotherapy in major depressive disorder: Clinical outcomes and predictors from a large naturalistic study. Brain Stimulation. doi: https://doi.org/10.1016/j.brs.2017.11.004
2) Iseger, T. A., Padberg, F., Kenemans, J. L., Gevirtz, R., & Arns, M. (2017). Neuro-Cardiac-Guided TMS (Heart-Brain Coupling): Probing DLPFC-sgACC-vagus nerve connectivity using heart rate-first results. Brain Stimulation. doi: http://dx.doi.org/10.1016/j.brs.2017.05.002
Brainclinics active at Brain Stimulation conference in Barcelona
Brainclinics active at Brain Stimulation conference in Barcelona
Researchers from research institute Brainclinics will present new data at the Brain Stimulation conference in Barcelona. Tabitha Iseger will present data that validate the proof-of-concept behind the new Neuro-Cardiac-Guided TMS (Heart-Brain Coupling) approach. This method could potentially become a new way to more reliably identify the right cortical locations for rTMS stimulation in the treatment of depression. Lana Donse will present some first clinical results on rTMS treatment in Obsessive Compulsive Disorder (OCD), association with sleep problems and predictors for treatment response to rTMS.
Neuro-Cardiac Guided TMS (NCG TMS)
Autonomic regulation is disturbed in depressed patients. Depressed patients express a higher heart rate and a lower heart rate variability (HRV), which is more pronounced in patients with severe MDD. HRV is the variability in heart rate due to external cues, as, for example, respiration. This indicates that the heart is connected to the brain network that is implicated in MDD. Indeed, several studies show connectivity between the brain structures involved in this network (DLPFC, sgACC, vagal nerve) and the heart. Moreover, some research indicates that rTMS treatment leads to heart rate decreases, thus a normalization of heart rate after treatment.
This connectivity can thus be used to validate whether the network is correctly targeted with rTMS. Since the heart is involved, correct targeting of, for example, the DLPFC, should lead to heart rate decreases. If it’s not, the DLPFC might not be targeted accurately. In common rTMS practice, the DLPFC is found according to the 5 (or 6) cm rule (5cm anterior from the place where thumb movement is found), or using the BEAM-F3 method. This is adequate on the group level, but individually there might be substantial variation. Ten healthy subjects received 3 X 5sec. trains of 10Hz TMS on 3 different scalp locations on the left (F3, FC3 and C3), and 3 locations right (F4, FC4 and C4), while their ECG was recorded. The ECG was converted into R-R interval data. As expected, on the group level, the largest HR decrease was observed for both F3 and F4. This is where, in theory, the DLPFC is located. However, substantial inter-individual variability was observed. For some subjects, the location that showed the largest HR decrease was FC3 or FC4. This indicates that for those subjects, the DLPFC might be located more towards FC3 or FC4. The DLPFC is the rTMS target for depression, and targeting it more accurately, could improve clinical response rates in depression. Moreover, the stimulation output might be lowered due to the higher specificity, and rTMS treatment will be better tolerable. This study thus confirms the earlier proposed concept of Neuro-Cardiac Guided TMS (NCG TMS).
Download the poster by Tabitha Iseger here (Neuro-Cardiac Guided TMS, NCG TMS)
Sleep disturbances in OCD: Association with non-response to rTMS
A group of 22 patients received at least 10 sessions of rTMS. Firstly, rTMS treatment was successful in more than half of the patients, with a response rate of 55%. Responders showed a strong reduction in both OCD and depression symptoms. Secondly, responders and non-responders showed differences in symptoms of sleep disorders, with a larger severity in non-responders. More specifically, symptoms of circadian rhythm sleep disorder could accurately discriminate non-responders from responders. These symptoms could therefore indicate differences in underlying mechanisms, and may be used as a predictor of non-response to rTMS in OCD.
Download the poster by Lana Donse here (Sleep, rTMS and OCD)
Brainclinics presents new scientific results at IPEG conference
Brainclinics presents new scientific results at IPEG conference
At October 26-30, researchers from Research Institute Brainclinics have presented the latest results of ongoing research at the International Conference of “the International Pharmaco-EEG Society (IPEG)", which took place in Nijmegen, The Netherlands this time.
During this successful, well attended (160 visitors from 24 different countries), meeting the following topics were presented by Brainclinics:
- Dr. Martijn Arns presented the current status of personalized medicine and new results from the latest treatment prediction studies for depression and ADHD.
- Drs. Berrie Gerrits showed promising results demonstrating that people who have good attention activated a specific brain network in a different way than people with poor attention. Interestingly, adults with ADHD showed the same pattern as healthy people with poor attention.
- Dr. Madelon Vollebregt demonstrated the importance of doing research into alpha brain waves in relation to ADHD. These waves were not clearly seen in the back of the head in boys with ADHD in contrast to in healthy boys. In addition, these brain waves were slower in the front of the head in adults with ADHD who did not respond to the drug methylphenidate (better known by the brand name Ritalin or Concerta) than those who did respond.
- Also, Madelon presented a study in which a relationship was demonstrated between the change of sunlight in the period after birth, and the number of attentional errors made in adulthood by people with specific risk gene also associated with ADHD (DRD4 7R genotype).
- Drs. Tabitha Iseger presented results of the iSPOT-D-study in which it was found that direct stimulation of a brain network comprising the brain regions' dorsolateral prefrontal cortex (DLPC), and 'subgenuale anterior cingulate' (sgACC) leads to a reduced connectivity in alpha brain waves, specifically in men who responded well to the treatment. She also presented an introduction to Neuro-Cardiac-Guided rTMS (NCG rTMS); a method which seeks to stimulate using rTMS the above-mentioned network (as a substitute for the currently used "motor threshold' for the DLPFC) via the relationship between this network and changes in heart rate.
- Drs. Lana Donse presented the clinically very relevant result that sleep problems that occur in an obsessive-compulsive disorder (OCD), can predict the extent to which rTMS treatment will work in OCD patients.
- Finally, Drs. Nikita van der Vinne presented preliminary results of a meta-analysis -an analysis in which all studies on that topic so far are merged to one study- on alpha asymmetry as characteristic for depression. The trials that were included so far, although the phenomenon has often been adopted as fact, did not show evidence for a diagnostic value of alpha asymmetry for depression. Note that this finding is independent of the predictive value that can deliver alpha asymmetry for treatment.
- Dr. Sebastian Olbrich, a colleague from Zürich with whom Brainclinics closely cooperates, presented treatment prediction studies for depression and obsessive-compulsive disorder and explained the use of an EEG analysis program (LORETA).
Martijn, Madelon, and Sebastian were in the organizing committee of this conference. Madelon (secretary) and Sebastian (president) are part of the board of the organization and Martijn (former Treasurer) has handed down his duties after many years of involvement. The next meeting of the IPEG will take place in 2018 in Zürich.
All abstracts of IPEG presentations can be found online.
Brain activity predicts personalized antidepressant treatment
Brain activity predicts personalized antidepressant treatment:
Implications for male-female differences
Nijmegen, July 17th, 2015 – Today results from the large multicenter randomized iSPOT-D study were published in Clinical Neurophysiology demonstrating that brain activity can assist in predicting antidepressant treatment outcome to commonly used antidepressant drugs. In addition, this study clearly demonstrated qualitative differences in brain activity between males and females with depression, with implications for predicting antidepressant treatment outcome.
An international group of researchers including researchers from Research Institute Brainclinics and Utrecht University published results from the international multicenter iSPOT-D study (international Study to Predict Optimized Treatment in Depression). This study recruited 1008 patients with a depression who were randomized to three different commonly used antidepressants and 336 non-depressed individuals. The researchers measured brain electrical activity, also called EEG or QEEG. When looking at differences in brain activity between depressed patients and controls, only small differences were found, not suitable for diagnostic purposes. However, most analyses suggested qualitative differences in brain activation patterns for males and females with depression (see box on the right), where males with a depression had decreased ‘alpha’ brain activity on the back portion of the brain, and females had increased ‘alpha’ brain activity on the frontal part of the brain.
Predicting personalized antidepressant treatment
The main aim of the study was to investigate if brain-based ‘biomarkers’, such as QEEG could predict treatment response. This study demonstrated that using a single biomarker – namely frontal alpha asymmetry – was able to predict treatment response and remission to escitalopram and sertraline (both belonging to the class of SSRI’s) for females only. This biomarker did not differ for the SNRI venlafaxine-XR nor for depressed males. A simulation demonstrated that when using this single biomarker to guide patients to an SSRI vs. an SNRI based on their individual brain activity, remission rates would have increased from 46% to 60% (an effective improvement in remission rate of 30%). “… the most surprising and promising aspect of this study is that the individual depressed patient can now be guided towards the most suitable treatment with a substantial improved chance for remission…’ said Martijn Arns, first author on the study. When replicated, this biomarker – possibly used in conjunction with other biomarkers identified in the iSPOT-D study – could help assist in the future of Personalized Medicine, where biomarkers are used to objectively guide patients to the right treatment.
Reference:
Arns, M., Bruder, G., Hegerl, U., Spooner, C., Palmer, D. M., Etkin, A., Fallahpour, K., Gatt, J.M., Hirshberg, L. & Gordon, E. (2015). EEG alpha asymmetry as a gender-specific predictor of outcome to acute treatment with different antidepressant medications in the randomized iSPOT-D study. Clinical Neurophysiology. doi:http://dx.doi.org/10.1016/j.clinph.2015.05.032
Note: This study was sponsored by Brainresource Ltd. But data-analysis and reporting were unconstrained.
Association between ADHD and intensity of sunlight
Association between ADHD and intensity of sunlight: Can ADHD be prevented?
Nijmegen, October 21st, 2013 – A study published today in Biological Psychiatry (Do Sunny Climates Reduce ADHD?) sheds new light on the increasing rates (prevalence) of attention-deficit/hyperactivity disorder, known as ADHD. Children with ADHD have problems with inattention, distractibility, disorganization, impulsiveness, and overactivity. This study found that “sunny” regions with high solar intensity, such as the US states of California, Arizona, and Colorado, and countries like Spain and Mexico have lower prevalence of ADHD. An apparent protective effect of sunlight accounted for 34-57% of the variance in ADHD prevalence. The authors speculate that this may be related to sunlight’s effects on preventing circadian rhythm (“biological clock”) disturbances. These results suggest ways to prevent or treat ADHD for a substantial sub-group of patients.
Researchers from Utrecht University, Research Institute Brainclinics, Leiden University, and Ohio State University today published their work suggesting a possible preventive effect of sunlight on ADHD. Examining ADHD prevalence rates per US state (CDC data, see figure 1a) and solar intensity maps (NREL data, see figure 1b) the authors observed a striking geographical coincidence between low ADHD prevalence and high solar intensity. Solar intensity is a measure of how much sunlight a specific area receives (in kWh/m2/day), often used for calculating how much energy solar panels will generate.
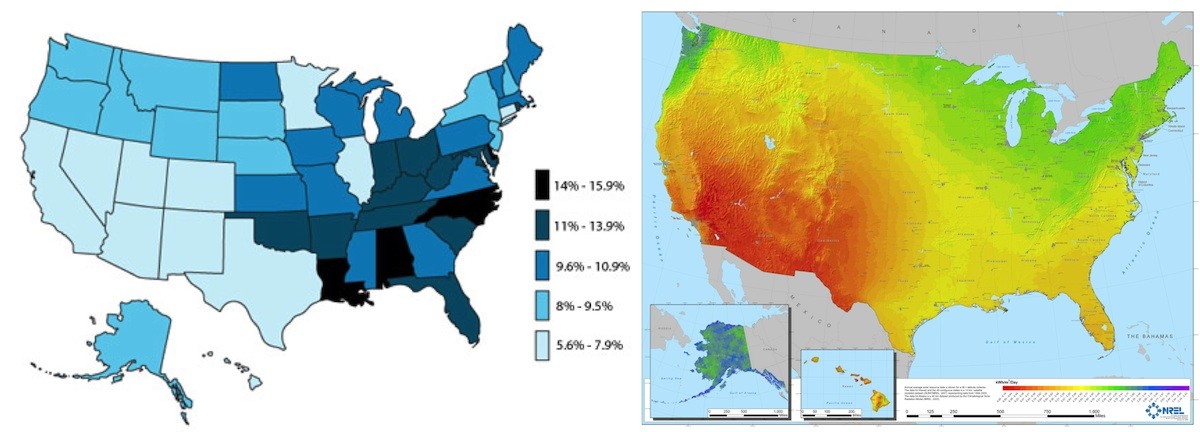
Figure 1a: ADHD Prevalence (CDC, 2003) Figure 1b: Solar-Intensity (NREL)
Based on this initial observation, the researchers further investigated this in 2 US and one non-US datasets, where they found a clear negative dose-response effect between solar intensity and the prevalence of ADHD. Considering all data, solar intensity accounted for 34-57% of the variation in ADHD prevalence. Many potential confounding factors were adjusted for in their analysis such as socio-economic status, low birth weight, infant mortality, geographical latitude, ethnicity/race, etc. However, these factors could not explain the results.
ADHD and sleep
Many patients with ADHD suffer from sleep problems, most often a difficulty falling asleep (or sleep-onset insomnia). For more information also see Sleep and ADHD. Shorter sleep duration and sleep restriction are associated with attention problems. The authors suggest that sleep disturbances may explain the attention problems in this subgroup of ADHD patients. Difficulty falling asleep has been linked to circadian rhythm problems (disturbances of the biological clock) and a delayed melatonin response. It is well known that sunlight is the strongest influence on the human biological clock. The authors hypothesize that this delayed circadian rhythm and difficulty falling asleep may be caused by increased evening use of modern media, such as tablet computers and smart phones, especially with social media increasing the exposure to such blue-light* sources during the evening. The authors speculate that strong sunlight during the day might reset the biological clock and act as an antidote to the evening exposure to artificial blue light causing sleep onset problems. The implications of these findings are that future research in ADHD should take into account sleep and circadian issues. From the public health perspective, manufacturers of tablets, smartphones and PCs could investigate the possibility of time-modulated color-adjustment of screens, to prevent unwanted exposure to blue light in the evening (e.g. f.lux software). Finally, these results could point the way to prevention of a sub-group of ADHD, by increasing the exposure to natural light during the day in countries and states with low solar intensity. For example, skylight systems in classrooms and scheduling playtime in line with the biological clock could be explored further.
* It is known that only 464-484 nm blue light specifically affects the biological clock, incandescent lamps have a low proportion of light in this range, whereas screens and some LED lights have a higher proportion in this range.
Reference: Arns, M. van der Heijden, K.B., Arnold, L.E. & Kenemans, J.L. (2013) Geographic variation in the prevalence of ADHD: The Sunny perspective. Biological Psychiatry DOI: 10.1016/j.biopsych.2013.02.010
Do Sunny Climates Reduce ADHD?
Do Sunny Climates Reduce ADHD?
Today the below press-release was distributed by Elsevier titled 'Do Sunny Climates Reduce ADHD?' about our study published in Biological Psychiatry.
Attention-deficit/hyperactivity disorder, or ADHD, is the most common childhood psychiatric disorder. Scientists do not know what causes it, but genetics play a clear role. Other risk factors have also been identified, including premature birth, low birth weight, a mother's use of alcohol or tobacco during pregnancy, and environmental exposures to toxins like lead.
ADHD is characterized by an inability to focus, poor attention, hyperactivity, and impulsive behavior, and the normal process of brain maturation is delayed in children with ADHD. Many individuals with ADHD also report sleep-related difficulties and disorders. In fact, sleep disorder treatments and chronobiological interventions intended to restore normal circadian rhythms, including light exposure therapy, have been shown to improve ADHD symptoms.
Estimates suggest that the average worldwide prevalence of ADHD ranges from about 5 to 7%, but it also varies greatly by region. A simple visual comparison of data maps released by the U.S. Centers for Disease Control and Prevention and the U.S. Department of Energy that display ADHD prevalence rates by state and solar intensities (sunlight) across the country, respectively, reveals an interesting pattern indicative of an association. So does this mean that there could be an identifiable relationship between ADHD prevalence rates and the sunlight intensity levels of particular regions?
The accumulation of these points led Dr. Martijn Arns and his colleagues to systematically and scientifically investigate this question. They collected and analyzed multiple data-sets from the United States and 9 other countries. Reporting their findings in the current issue of Biological Psychiatry, they did find a relationship between solar intensity and ADHD prevalence.
Even after controlling for factors that are known to be associated with ADHD, both U.S. and non-U.S. regions with high sunlight intensity have a lower prevalence of ADHD, suggesting that high sunlight intensity may exert a 'protective' effect for ADHD.
To further validate their work, they also looked at this same relationship with autism and major depressive disorder diagnoses. They found that the findings were specific to ADHD, with no associations observed between the other two disorders.
"The reported association is intriguing, but it raises many questions that have no answers," commented Dr. John Krystal, Editor of Biological Psychiatry. "Do sunny climates reduce the severity or prevalence of ADHD and if so, how? Do people prone to develop ADHD tend to move away from sunny climates and if so, why?"
As with all scientific research, further work is necessary, including a prospective replication of these findings. It is also important to realize that this data reflects only an association - not a causation - between ADHD and solar intensity levels so worried parents should not start planning cross-country moves.
However, these findings do have significant implications, explains Dr. Arns. "From the public health perspective, manufacturers of tablets, smartphones and PCs could investigate the possibility of time-modulated color-adjustment of screens, to prevent unwanted exposure to blue light in the evening."
"These results could also point the way to prevention of a sub-group of ADHD, by increasing the exposure to natural light during the day in countries and states with low solar intensity. For example, skylight systems in classrooms and scheduling playtime in line with the biological clock could be explored further."
The article is "Geographic Variation in the Prevalence of Attention-Deficit/Hyperactivity Disorder: The Sunny Perspective" by Martijn Arns, Kristiaan B. van der Heijden, L. Eugene Arnold, and J. Leon Kenemans (doi: 10.1016/j.biopsych.2013.02.010). The article appears in Biological Psychiatry, Volume 74, Issue 8 (October 15, 2013), published by Elsevier.
Sleep-improvement working mechanism neurofeedback ADHD
Sleep-improvement as a working mechanism for neurofeedback treatment in ADHD
Brain-activity of healthy children more ‘drowsy’ across last decade.
Nijmegen, November 12th, 2012 - Difficulty falling asleep and staying asleep are common symptoms in patients with ADHD, and these sleep complaints are often associated with attention and impulsivity problems, researchers from Utrecht University and research institute Brainclinics conclude in the scientific journal Neuroscience and Biobehavioural Reviews. The researchers in this article propose a neuro-anatomical model of neurofeedback, where neurofeedback results in falling asleep faster and better being able to maintain sleep, through an effect on so-called ‘sleep spindles’. At the same time, according to another study published in the Journal of Attention Disorders, over the last 10 years the brain activity of healthy children has become ‘drowsier’. This is most likely related to the fact that children sleep less, when compared to 10 years ago.
ADHD and sleep
Patients with ADHD often suffer from sleep problems, most often a difficulty falling asleep and maintaining sleep, but sometimes also more severe sleep problems such as sleep apnea (breathing problems) and restless legs syndrome. Specific treatment in ADHD subgroups with these two specific sleep disorders (apnea and restless legs syndrome) have been demonstrated to result in a greater reduction of ADHD symptoms compared to traditional ADHD treatment with medication (Ritalin). All these sleep disorders have in common a chronic reduction in the number of hours slept. Shorter sleep duration and sleep restriction have been clearly associated with attention problems and hence are suggested to explain the attention issues in these ADHD sub-groups. Furthermore, brain activity in ADHD patients during the day exhibit clear signs of drowsiness. Another study just published in the Journal of Attention Disorders found that healthy children over the last 10 years also exhibit more and more of these drowsiness brainwave patterns (Arns, Conners & Kraemer, 2012). Perhaps this also explains the increased ADHD prevalence in recent years. Of course, sleep problems are not the underlying problem in all ADHD patients, but at least in a substantial number of patients.
Neurofeedback, ADHD and sleep
Recent research suggests that neurofeedback has favorable and lasting treatment effects in ADHD. In neurofeedback a specific brain activity is trained and until recently it was unclear how this technique results in behavioral improvements in ADHD. Arns and Kenemans (2012) suggest that neurofeedback impacts on the brain system that becomes active during sleep, and is responsible for the generation of so-called "sleep spindles". Several studies have demonstrated that after application of neurofeedback during the day, the brain activity during sleep is altered. This change consists of an increase in sleep spindles, resulting in faster sleep onset times and improved sleep maintenance. Arns and Kenemans suggest that specifically these improvements in sleep can be seen as the cause of the effectiveness of neurofeedback in ADHD.
References
(also see the community )for articles
Arns, M. & Kenemans, J. L. (2012). Neurofeedback in ADHD and insomnia: Vigilance stabilization through sleep spindles and circadian networks. Neuroscience & Biobehavioral Reviews. doi:10.1016/j.neubiorev.2012.10.006
Arns, M. Conners, C. K. & Kraemer, H. C. (2012). A decade of EEG theta/beta ratio research in ADHD: A meta-analysis. Journal of Attention Disorders. doi:10.1177/1087054712460087
Doubling of Neurofeedback efficacy in ADHD treatment
Doubling of Neurofeedback efficacy in ADHD treatment
First study investigating personalized treatment in ADHD
Nijmegen, March 27, 2012 – A personalized treatment approach, tailoring Neurofeedback treatment to the individual ADHD patient almost doubled the effectiveness for attentional and hyperactivity/impulsivity problems. These results have just been published in the scientific journal ‘Applied Psychophysiology and Biofeedback’. This study is the first scientific study investigating whether personalizing Neurofeedback treatment, based on a so-called quantitative EEG or QEEG, results in a higher effectiveness of this treatment in ADHD.
Several scientific studies have already demonstrated that neurofeedback treatment has beneficial and lasting effects in the treatment of ADHD (Arns et al, 2009). A new development in psychiatry is that of 'tailor-made treatments' sometimes referred to as ‘personalized medicine’. This development is becoming more and more popular due to the fact that most ‘conventional’ treatments in psychiatry have demonstrated limited efficacy. The development of personalized medicine therefore focuses more on providing the right treatment for the right person in order to achieve a more effective treatment outcome. In a study conducted by Research Institute Brainclinics, neurofeedback protocols were tailored to the individual patient. On the basis of patients’ individual quantitative EEG – also called a QEEG - it was determined which well-investigated neurofeedback protocol was applied to a specific patient. Sixty-seven percent of patients responded well to this treatment (more than 50% reduction in symptoms). The reported "effect-size" of 1.8 (a measure of the magnitude and clinical relevance of the treatment effect) in this study was found to be almost double the effect-size as compared to previously reported studies. This treatment approach to Neurofeedback in the treatment of ADHD is also applied in practice at Brainclinics. These results were recently published in the international scientific journal Applied Psychophysiology and Biofeedback (Arns et al, 2012).
References:
Arns, M., Drinkenburg, W. H. I. M., & Kenemans, J. L. (2012). The effects of QEEG-informed neurofeedback in ADHD: An open label pilot study. Applied Psychophysiology and Biofeedback. doi:10.1007/s10484-012-9191-4
Arns, M., de Ridder, S., Strehl, U., Breteler, M., & Coenen, A. (2009). Efficacy of neurofeedback treatment in ADHD: The effects on inattention, impulsivity and hyperactivity: A meta-analysis. Clinical EEG and Neuroscience, 40(3), 180-9.
Outcome to treatment for depression predicted
Outcome to treatment for depression predicted
Magnetic brain stimulation (rTMS) effective treatment
Nijmegen, February 27, 2012 - Favorable treatment outcome in 78% of depressed patients after on average 21 sessions. These results were recently published based on the combination of magnetic brain stimulation (rTMS) and psycho-therapy in the treatment of depression. It was further demonstrated that by means of brain activity - or EEG research- it could be predicted which patients would respond and which patients would not respond to this treatment combination.
rTMS is an effective addition to psychotherapy
In a large multicenter study in 90 patients with depression the combination of magnetic brain stimulation (rTMS) with psychotherapy was investigated. This research was also intended to investigate whether it is possible to predict in advance which patients will and which patients will not respond to treatment. The combination of rTMS treatment with psycho-therapy resulted in a success rate of 78. On average, patients needed 21 treatments. These results were just published in the leading international scientific journal 'Brain Stimulation'.
Brain activity as a predictor of treatment outcome: Personalized Medicine
In this study it was also examined whether it was possible to predict treatment outcome based on brain function tests conducted before treatment was started. This development is also often referred to as 'personalized medicine'. Psychological factors and personality variables such as perceived anxiety, stress and depression were not found to predict treatment outcome to rTMS. However, specific brain activity markers (quantitative EEG or QEEG markers) assessed before treatment, demonstrated to be good predictors of the effects of this combined treatment. If this results can be prospectively confirmed in a new population, this could be applied in practice and implicate that in the future patients may be advised about the likelihood of success before treatment is initiated.
What is rTMS?
Repetitive Transcranial Magnetic Stimulation (rTMS) is a neuromodulation technique used in the treatment of depression. With this technique, an electro-magnetic coil is placed over the head. By means of a pulsating magnetic field, specific parts of the brain are stimulated with the goal to modulate blood flow and electrical activity in a specific part of the brain. Click here for more information on rTMS in the treatment of depression.
References:
Arns, M., Drinkenburg, W. H. I. M., Fitzgerald, P. B., & Kenemans, J. L. (In Press). Neurophysiological predictors of non-response to rTMS in depression. Brain Stimulation. doi: 10.1016/j.brs.2011.12.003
Brain research better predictor for treatment than behavior
EEG predicts right treatment for ADHD and depression,
Brain research better predictor for treatment than behavior
Antidepressants for people with depression and ritalin for ADHD patients. It is the usual medical treatments for such disorders. But the medication is not always effective for all patients. PhD student Martijn Arns conducted research into predicting the correct treatment method for depression and ADHD. According to him, EEG research offers a solution: "In the future, after a simple EEG examination, the patient could receive personalized treatment." Arns will be awarded a PhD by Utrecht University on December 23.
Treatments in psychiatry are often determined based on the behavior of the patient. For example, if hyperactivity and attention problems are observed in a patient, ADHD is diagnosed, after which the patient is prescribed the drug ritalin. However, the medication does not always appear to have the desired effect. According to PhD student Arns, that is hardly surprising: “Both depression and ADHD have different subtypes. Medication works for one variant, but not for the other."
Electrodes on the head
To see if a treatment method has a chance of success, PhD student Arns subjected his patients to an EEG. With an EEG the patient gets electrodes placed on the head so that the brain activity can be measured. After this EEG patients were prescribed one of the following three treatments: treatment with medication, with magnetic brain stimulation (rTMS) in depression or with neurofeedback in ADHD. After treatment, Arns examined whether there had been improvement in the patient and whether there was a relationship between the success of the treatment method and the EEG prior to treatment.
Ritalin positive for only one subgroup
Arns writes in his dissertation that he has distinguished three subgroups of ADHD patients. One of those subgroups is characterized by responding well to the drug ritalin. "For example, this group exhibited increased theta activity in the EEG: an activity that is associated with a lowered alertness level and reduced sustained attention." In depression, this increased theta activity was found to be associated with non-responding to antidepressants and rTMS. Possibly this subgroup of patients responds better to, for example, ritalin. Another important measure, the so-called slow alpha peak frequency, appeared to be a predictor for the general failure to respond to treatments for both ADHD and depression. "Future research must therefore focus on the development of new treatments for this substantial subgroup," says Arns.
Brain activity instead of behavior
In his dissertation, the Utrecht researcher argues for more use of personalized treatments in psychiatry. Thereby the behavior should no longer be taken as a starting point for a diagnosis and therefore for a treatment, but the measured brain activity. "A simple EEG examination would be a welcome tool for the psychiatrist."
Follow-up investigation
For a large-scale follow-up study in this area, patients with depression or ADHD are still looking for who are considering taking medication. For more information see also: iSPOT.
More information
You can download the thesis 'Personalized Medicine in ADHD and Depression: A quest for EEG treatment predictors' here.
Burnout syndrome visible in brain activity
Burnout syndrome visible in brain activity
For the first time, differences have been found in brain activity between healthy people and people suffering from burnout. A breakthrough. Until now, this condition was not to be determined on the basis of objective data. Nijmegen researchers found a combination of EEG changes that are unique to burnout. They have thus found an objective measure for the diagnosis of burnout.
A team of researchers led by Dr. Gilles van Luijtelaar of the Donders Institute for Brain Cognition and Behavior at Radboud University Nijmegen publishes the results in the recently published Journal of Neuropsychiatry and Clinical Neurosciences, the scientific journal of the American Neuropsychiatric Association.
Difficult diagnosis
Burnout is not recognized in all countries. Diagnosis is difficult, among other things, because some characteristics resemble those of depression and chronic fatigue (CFS). The disorder also has no place of its own in the standard work for diagnosis and treatment of mental disorders, the Diagnostic and Statistical Manual of Mental Disorders (DSM).
Strict pre-selection of burnout
With the help of EEG, the researchers recorded the brain activity of thirteen burnout patients and compared it with data from just as many healthy volunteers. A small group, but sufficiently reliable for a first study, says Van Luijtelaar. "A strict selection was made in advance. Our test subjects were without a doubt suffering from a burnout. Their problems were clearly work-related. Those with depressive symptoms and / or other psychiatric problems did not make the selection."
EEG of burnout patients is different
The test subjects participated in various neuropsychological and EEG tests. For example, spontaneous activity was measured in a relaxed state when the subjects quietly had their eyes open and closed. A nice rhythmic and balanced wave pattern was visible in both groups in the form of alpha waves (8-12 Hz waves, which mainly occur with relaxation). However, the peak frequency of this rhythm was lower in the burnout group. This points to a lower willingness or ability to make mental efforts.
The beta rhythm, the fast little brain waves associated with a waking state, were also smaller. According to the researchers, this points to reduced activation of the cortex, the outermost layer of the large brain. In burnout patients there were - unlike those in depression - no differences in frontal EEG activity between the left and right hemisphere.
A second test, in which the participants listened to a series of tones that was occasionally interrupted by a different tone, also showed clear differences between the two groups. Deviations were found in the P300, an excited brain wave. This wave was flatter with burnout patients: they responded less strongly to the abnormal tone. Such a flattened wave also occurs with depression, but unlike burned out patients, they do not have an early peak of the P300.
Comparisons with depression and CFS
Because some symptoms of depression and chronic fatigue are similar to those of burnout, the researchers compared parts of their measurements with results such as those described for depressives and CFS patients. The combination of the EEG changes found is unique for burnout. The researchers conclude from this that they have an objective measure - a biomarker - to be able to determine this condition.
Recognition burnout patients
"An important result," says neuroscientist Gilles van Luijtelaar. To him it's even more important that the research is published in an American journal. "In the US, burnout is not recognized as a disease. Now that psychiatrists are aware of this objective measure, patients will be recognized and treated better. " The authors do, however, emphasize that this is an initial study in a small group. The research - as it goes in science - needs a follow-up in a larger group.
Cooperation between practitioners and scientists
This study combines expertise from practitioners and scientists. Researchers from Donders Center for Cognition (Dr. Gilles van Luijtelaar, Dr. Martijn van den Bunt) and the Behavioral Science Institute (Dr. Ger Keijsers, Dr. Marc Verbraak) of Radboud University collaborated with the HSK Group, a national healthcare organization specialized in the diagnosis and treatment of mental disorders, including burnout (dr. Marc Verbraak) and Brainclinics Diagnostics (dr. Martijn Arns).
The patients were recruited via HSK. Clinical psychologists Dr. Ger Keijsers and Dr. Marc Verbraak know the symptoms of and the usual diagnosis for burnout and chose the most optimal selection criteria, in which patients with depression and CFS were filtered from the research group. Brainclinics Diagnostics provided the measurements and Martijn Arns, Martijn van den Bunt and Dr. Gilles van Luijtelaar drew up the experiment, edited the data and took care of the publication.
EEG Findings in Burnout Patients.
Gilles van Luijtelaar, Marc Verbraak, Martijn van den Bunt, Ger Keijsers, Martijn Arns. The Journal of Neuropsychiatry and Clinical Neurosciences, (Spring issue).
unique and effective treatment for depression
Conversation therapy and magnetic brain stimulation: unique and effective treatment for depression
Nijmegen, 28 August 2009 - The combination of conversation therapy and magnetic brain stimulation (rTMS) in the treatment of depression results in an effectiveness of 75% after an average of 20 sessions. These are the results of a scientific study that will be published this month. The addition of rTMS in talk therapy has the same purpose as antidepressants. rTMS has hardly any side effects, such as weight gain or sleeping problems. This therapy is no different from regular conversation therapy, but the addition of rTMS seems to make people more susceptible to dealing with the depression and therefore the long-term effect is often better.
rTMS effective addition to call therapy
The combination of conversation therapy and rTMS treatment, with a success rate of 75%, seems to be a golden handle for the treatment of depression. Between 8 and 12 sessions is the turning point for whether or not an effect. On average, clients undergo 20 treatments for a long-lasting result. The depression is tested with questionnaires at every 5th session. Initial results from research into the long-term effects show that after six months the depressive symptoms have still decreased significantly compared to the intake interview prior to treatment. The results of this study will be published this month in the "Journal of Neuropsychiatry and Behavioral Neurology".
What is rTMS?
Repetitive Transcranial Magnetic Stimulation (rTMS) is a neurophysiological technique that can be used for the treatment of various neurological disorders including depression and Parkinson's disease. With this technique an electromagnetic coil is placed on the head. By means of a pulsating magnetic field, specific parts of the brain are stimulated with the aim of increasing or decreasing blood flow and electrical activity in a specific part of the brain. These changes
in activity and blood flow can be accompanied by behavioral changes such as a decrease in depressive feelings.
Treatment is more accessible than people often think
As a first-line psychologist's practice, the psychologists at Brainclinics work, among other things, on the basis of cognitive behavioral therapy. The unique combination of conversation therapy and rTMS makes the treatment very effective, so that depression can be treated in a short time.
It is quite conceivable that rTMS will play an important role in the future
regular psychological assistance.
More information about the treatment can be requested via
Reference
rTMS bij Depressie (2009). Desiree Spronk & Martijn Arns. Tijdschrift voor Neuropsychiatrie en Gedragsneurologie, Juli-Augustus; 163-167
Neurofeedback Evidence-Based treatment for ADHD
New research shows: Neurofeedback is an ‘Evidence-Based’ treatment for ADHD
Nijmegen, July 16th 2009 – Neurofeedback – also called EEG Biofeedback – is a method used to train brain activity in order to normalize Brain function and treat psychiatric disorders. This treatment method has gained interest over the last 10 years, however the question whether this treatment should be regarded as an Evidence-Based treatment was unanswered until now. Tomorrow a study will be published in the scientific journal ‘Clinical EEG and Neuroscience’ demonstrating that Neurofeedback can indeed be regarded as an evidence-based treatment for Attention Deficit- / Hyperactivity Disorder (ADHD).
Neurofeedback is a treatment where real-time feedback is provided for specific brain activity (most often EEG) in order to learn the brain to suppress or produce specific brain activity. This method was initially discovered for the treatment of Epilepsy and from 1976 investigated further for the treatment of ADHD. This technique has become more popular by clinicians worldwide, and is currently provided for the treatment of several disorders. Critics have often questioned the efficacy of Neurofeedback and whether it can be considered an Evidence Based treatment or not.
In collaboration with researchers from Tübingen University (Germany), Radboud University (Nijmegen, the Netherlands), Brainclinics and EEG Resource Institute a so-called meta-analysis was conducted on all published research about Neurofeedback treatment in ADHD. This meta-analysis included 15 studies and 1194 ADHD patients. Based on this study – which will be published in the July issue of Clinical EEG and Neuroscience – it could be concluded that Neurofeedback can indeed be considered an Evidence-Based treatment for ADHD. The results show that neurofeedback treatment has large and clinically significant effects on Impulsivity and Inattention and a modest improvement of Hyperactivity. See below the abstract of this study.
These findings apply to Neurofeedback treatment for ADHD, but do not automatically imply that Neurofeedback can be considered evidence based for any disorder. The efficacy of Neurofeedback has to be assessed separately for each disorder. For example, a meta-analysis of EEG biofeedback in Epilepsy is published in the same issue of EEG and Clinical Neuroscience demonstrating clinical efficacy in the treatment of epilepsy.
Interested clients are advised to make an informed choice regarding Neurofeedback therapists, since there is a large heterogeneity in neurofeedback treatment approaches and clinicians. It is advised to look for psychologists or physicians who are at least a member of a professional organization such as the International Society for Neurofeedback and Research (ISNR: www.isnr.org) or other professional organizations and who use investigated methods.
Literature
Arns, M. (2011). Personalized medicine in ADHD and depression: A quest for EEG treatment predictors. PhD thesis, Utrecht University.
Arns, M., de Ridder, S., Strehl, U., Breteler, M. & Coenen, A. Efficacy of Neurofeedback Treatment in ADHD: The effects on Inattention, Impulsivity and Hyperactivity: a Meta-Analysis. Clinical EEG and Neuroscience; 40(3), 180-189.
Arns, M. (2008) Personalized Medicine: Nieuwe ontwikkelingen in de diagnostiek en behandeling van Depressie en ADHD. De Psycholoog, September 2008.
Efficacy of neurofeedback treatment in ADHD: The effects on inattention, impulsivity and hyperactivity:
A meta-analysis.
Martijn Arns 1,2,*, Sabine de Ridder 2, Ute Strehl 3, Marinus Breteler 4, 5 & Anton Coenen 5
1 Brainclinics Diagnostics, Nijmegen, The Netherlands
2 Brainclinics Treatment, Nijmegen, The Netherlands
3 University of Tuebingen, Germany
4 EEG Resource Institute, Nijmegen, The Netherlands
5 Radboud University, Nijmegen, The Netherlands
ABSTRACT
Since the first reports of neurofeedback treatment in ADHD in 1976 many studies have been carried out investigating the effects of neurofeedback on different symptoms of ADHD such as inattention, impulsivity and hyperactivity. This technique is also used by many practitioners, but the question as to the evidence-based level of this treatment is still unclear. In this study selected research on neurofeedback treatment for ADHD was collected and a meta-analysis was performed.
Both prospective controlled studies and studies employing a pre- and post-design found large effect sizes (ES) for neurofeedback on impulsivity and inattention and a medium ES for hyperactivity. Randomized studies demonstrated a lower ES for hyperactivity suggesting that hyperactivity is probably most sensitive to non-specific treatment factors.
Due to the inclusion of some very recent and sound methodological studies in this meta-analysis potential confounding factors such as small studies, lack of randomization in previous studies and a lack of adequate control groups have been addressed and the clinical effects of neurofeedback in the treatment of ADHD can be regarded as clinically meaningful. Three randomized studies have employed a semi-active control group which can be regarded as a credible sham control providing an equal level of cognitive training and client-therapist interaction. Therefore, in line with the AAPB and ISNR guidelines for rating clinical efficacy, we conclude that neurofeedback treatment for ADHD can be considered ‘Efficacious and Specific’ (Level 5) with a large ES for inattention and impulsivity and a medium ES for hyperactivity.
Keywords: Neurofeedback, EEG Biofeedback, ADHD, meta-analysis, inattention, impulsivity, hyperactivity.
International Biomarker-Depression study: iSPOT-D
International Biomarker-Depression study: iSPOT-D
Nijmegen, 26 March 2009 - Research shows that antidepressants only affect 40-60% of patients, while painkillers work for almost everyone. How is this possible? And above all, how can this be improved? To answer these questions, Brainclinics Diagnostics has started an international partnership with the largest Biomarker study in Depression ever conducted. In total, almost 3000 people will be examined for genetic material, brain activity and psychological variables. In the Netherlands this investigation will officially start on 1 April. The aim of this research is to arrive at biomarkers - indicators that can be used to estimate whether or not someone will benefit from a certain antidepressant.
Around 850,000 people in the Netherlands currently suffer from depression (RIVM). The prognosis is that this number will increase sharply in the coming period. The World Health Organization predicts that depression will be the number two public illness in 2020. In most cases, antidepressant medication is prescribed. Currently there are almost 1 million people in the Netherlands who use antidepressants. Research shows that a limited proportion of patients have an adequate effect of antidepressant medication, only 40-60%. What is the reason for that?
Previous research shows that there are different neurophysiological sub-types of depression within the group of patients. This is probably the explanation that one patient does and another does not respond well to antidepressants. These subtypes can be distinguished by biomarkers including EEG, genetic material and neuropsychological tests. To further investigate this, the Brain Resource Company started the iSPOT-D study (international Study to Predict Optimized Treatment response in Depression). In this study, almost 3000 people will be investigated worldwide in which brain activity (QEEG and fMRI), genetic material (DNA) and (neuro) psychological measurements are mapped out, before and during the use of antidepressant medication. This research is also part of a new development in psychiatry: Personalized Medicine.
The iSPOT-D study will provide more insight into the clinical picture of depression. Above all, the aim of this research is to identify biomarkers that can predict which medication can best be prescribed for which patient before starting treatment. This would mean a huge improvement in the treatment of depression.
In the Netherlands, this investigation will formally start on 1 April. This research is conducted by Brainclinics Diagnostics B.V. in Nijmegen. The research has now been opened for depression patients who will be treated with antidepressants, but who have not yet started to do so.
Literature
Arns, M. (2008) Personalized Medicine: Nieuwe ontwikkelingen in de diagnostiek en behandeling van Depressie en ADHD. De Psycholoog, September 2008.
Gordon, E. (2007) Integrating genomics and neuromarkers for the era of Brain-related Personalized medicine. Personalized Medicine, 4:201-215.
Also see https://brainclinics.com/personalized-medicine/
the Personalized Medicine section for background information.
